Tag East grinstead
19 Apr
Heel Pain (Plantar fasciitis)
Heel Pain (Plantar Fasciitis) Introduction Heel pain is a very common problem that may be attributed to several etiologies, including heel spurs, plantar fascia irritation (acute or chronic), and bursitis. Plantar fasciitis is thought to result from microtears in the fascia due to repeated biomechanical stress on the arch of the foot on weight-bearing. Plantar fasciitis is an inflammation of the plantar fascia & the perifascial structures. Chronic stress to the origin of this fascia on the calcaneus may cause calcium to deposit, forming a spur (plantar calcaneal spur). Plantar Fascia is a Dense, broad band of connective tissue attaching proximal and medially to the calcaneus and fans out over the plantar aspect of the foot and works in maintaining the stability of the foot and bracing the longitudinal arch. The pain is maximal when the patient first stands in the morning and tends to decrease with walking. Ten percent of people may experience pain under the heel (plantar heel pain) at some time during their life. Cause Plantar fasciitis is the most common cause of heel pain in the adult population with an incidence of around 10%. It affects adults across the age spectrum with an incidence in women twice that of men. Ethnicity does not influence incidence. There is a higher preponderance in those who play sport either recreationally or professionally. Increased body weight and an increased body mass index (BMI) have also been shown to be significant risk factors for developing plantar fasciitis. Pregnancy, flat feet, high arched feet, poorly fitting or worn footwear, Calf muscle tightness, gait abnormalities, prolonged standing, running, jumping and walking are additional contributory factors. Excessive lumbar lordosis—a condition in which an increased forward tilt of the pelvis produces an unfavourable angle of foot strike when there is a considerable force exerted on the ball of the foot—can also contribute to this problem. Running on soft surfaces are also potential causes of plantar fasciitis. Clinical features Assessment Looking for Swelling, Arches, Deformity, Gait, posture, tenderness, Tight Structures etc & History Summary For the treatment of heel pain or plantar fasciitis, research has not indicated any consensus on a specific treatment regimen that has proven to resolve heel pain with any statistical significance. However nonsurgical treatment is ultimately effective in approximately 90% of patients. It is equally important to correct the problems that place individuals at risk for plantar fasciitis, such as the increased amount of weight-bearing activity, increased intensity of activity, hard walking/running surfaces and worn shoes. Early recognition and treatment usually lead to a shorter course of treatment as well as an increased probability of success with conservative treatment measures S.M.A.R.T. approach to prevent plantar fasciitis The Canadian Physiotherapy Association (CPA) Calf and Achilles stretching is achieved by performing asymmetrical stretching exercises ANRC Phases of Rehabilitation Phase 1- Pain Relief (Trigger Point Therapy, Myofascial Release, Sports massage, Taping, Electrotherapy modalities, Postural Correction, Basic Home exercises etc) Phase 2- Restoration of Range of movement and muscle length (Stretches, Exercises for the small muscles of the foot, Postural training, Basic Strength Training, Orthotics if needed) Phase 3- Maintenance Phase & Improve the activity of daily living (Intensive Strength Training, Ergonomic Modifications in Sports & Daily Activities Reference
READ MORE17 Oct
Importance of pelvic floor strengthening exercises re-emphasised
UK physiotherapists used Valentine’s Day to launch a campaign to encourage members of the public to perform physiotherapy exercises to tighten up their pelvic floors. Pelvic floor muscle exercises tone and strengthen these muscles, improving blood supply and nerve activity, all leading to greater pleasure. Many people are already aware of the importance of tightening the Kegel muscles – those used to stop urine mid-flow – in order to tighten the pelvic floor, but the campaign highlights that it’s also important to practice tightening the muscles around the anal sphincter too. Studies have shown that doing this can assist in bringing the vaginal walls together for women, while it can also help men to sustain an erection. In addition, the campaign emphasises the importance of relaxing the muscles after each contraction and suggests fitting in these exercises while performing other activities, such as brushing teeth. Experts recommend squeezing these muscles ten to 15 times in a row at least once a day and that each squeeze should be short and powerful. Varying the strength of contractions is also important; physios suggest trying to maintain a squeeze for five to ten seconds regularly too, while continuing to breathe normally. (Article from Just Physio)
READ MORE2 Sep
No, I am not just living with fibromyalgia..!!
No, I am not just living with fibromyalgia..!! No, I am not just living with fibromyalgia – I am living my life to the fullest – and to be honest much better than most people around me! I was diagnosed with fibromyalgia in Apr 2008, almost a full year after I first experienced debilitating pain in my right leg. By the time I found a doctor who could tell me what was wrong with me, it was full blown – I was in pain 24 hours a day and no part of my body was spared – arms & legs, upper back, lower back, even abdomen!!! The initial treatment plan included oral medication and 5 days of physical therapy. My idea of physical therapy was heated packs, infrared and ultrasound treatments. I had absolutely no idea what lay in store for me. As I landed at the clinic for my first session of physical therapy, Praveen TJ (my first physiotherapist) asked me a few questions about my pain type – where, what kind, how strong etc. Then he started “giving” me trigger point therapy – this involves manually pressing trigger points on muscles to reduce the pain. Fibromyalgia causes a heightened feeling of pain when pressure is applied and here I was paying to have that pressure applied to the most painful area – trigger points! After 5 days of this painful therapy, I consulted the doctor again, as planned, and he prescribed me one month of therapy. That’s when I knew that I am not getting rid of this problem anytime soon and I might as well try to understand the problem and the treatment course a little better. So I started asking questions – to doctor, to Praveen, to other physiotherapists at the clinic, to anyone who was willing to answer my questions- as Praveen used to call me – I was a walking talking “question bank”. Slowly I understood a few but very important things like – what is referred pain; what is the difference between trigger point pain and tenderness pain; what is a myofascial pain; what activities, especially if repeated, would increase pain in which area of my body. A month got over, the relief was there but not enough so I started taking one hour of physical therapy every day. During this time my fitness levels also took a nosedive. I had to stop all forms of exercising including yoga as that was increasing my pain and undoing the work done by my therapist. A few more months went by and the therapy became part of my routine – wake up, go to work, leave work, go to the clinic, reach home, apply hot pack, have dinner and have restless sleep (thanks to fibromyalgia). As luck would have it, things took a turn for the worse. By Dec 2008, while the pain had come down, I had started to feel very tired and fatigued- so much so that I would lie down at the back seat of my car while I was driven to work. (Due to severe pain I had stopped driving almost a year back). And suddenly I started gaining weight as well – that too at the rate of 6 pounds a month. This weight gain was a result of severe thyroid inactivity – my TSH levels were 160 (normal is less than 5.5.) We found antithyroid antibodies in my blood, proof that my own immune system was killing it – for that matter had already killed it (hence the super crazy TSH levels). At this time I also tested positive for antibodies linked to fibromyalgia – establishing the fact that the two conditions were inter-related and that both were autoimmune diseases. Amidst all this chaos, in a rare moment of sanity, I decided to try meditation. I signed myself up for a 10-day residential course on the outskirts of the city and without thinking landed there. In hindsight, had I thought a lot about it I would not have attended the course. The course helped me stop using food and alcohol for emotional comfort – the first step towards recovery! I stopped gaining more weight and started thinking about how to shed the 40 pounds that I had gained and get my life back. While the doctor was still against me exercising, Praveen said that we would start slowly and that he will help manage the pain with therapy. Under his guidance, I started incline walking on the treadmill and as expected the pain did go up but with extra therapy and my determination and his motivational words, I kept increasing the incline and speed and distance walked. There were many times when I felt discouraged either because of pain or when I would think of how I used to run at high speeds for an hour or so before fibromyalgia, but I didn’t stop working out. First I increased the time to 20 minutes, and then I increased the incline, then the speed and then time again …and in a few weeks, I was walking for 30 minutes at 6 mph at an incline of 10. For another 3 years, I stayed on this course, walking on incline, yoga, physical therapy and meditation. It had been 4.5 years since the pain started and I had tried various alternative remedies as well – Homeopathy, Ayurveda, Naturopathy, Acupressure, Acupuncture and of course was still on Amitriptyline and physical therapy. I still didn’t know the root cause of fibromyalgia (actually no one still knows for sure what causes it- some say it’s genetic, some say is just stress, some say it’s environment) and hence couldn’t attack it. Only thing I had realized was that therapy and medication alone will not cure me. Then I learned that trigger point therapy kind of weakens muscles and in turn, weakened muscles develop trigger points easily. So more therapy I took, more I increased the probability of fresh trigger points. The only way out of this
READ MORE6 Apr
What is iliotibial band syndrome and how is it treated?
Iliotibial (IT) band syndrome is often caused by repetitively bending the knee during physical activities, such as running, cycling, swimming, and climbing. The IT band is a group of fibers that run the length of the upper leg, from the hip to the top of the shin.The best treatment is often to stop doing the activity that is causing the pain. In more severe cases, surgical options may need to be considered. Symptoms 1) Pain when running or doing other activities involving the outside of the knee2) A clicking sensation where the band rubs against the knee3) Lingering pain after exercise4) The knee is tender to touch5) Tenderness in buttocks6) Redness and warmth around the knee, especially the outer aspect Treatment IT band syndrome is often relatively easy to treat. There are two main types of treatment for the condition: 1) Reducing pain and swelling2) Stretching and preventing further injury Some of the most common ways to treat IT band syndrome include: 1) Resting and avoiding activities that aggravate the IT band2) Applying ice to the IT band3) Massage4) Anti-inflammatory medications, which are often available overthe counter5) Ultrasounds and electrotherapies to reduce tension (News from medical news today) Us our contact form or call today our ANRC Physiotherapy clinics in Horsham, East Grinstead, West Sussex or Lingfield, Surrey which Physiotherapy or Sports injury treatments.
READ MORE4 Apr
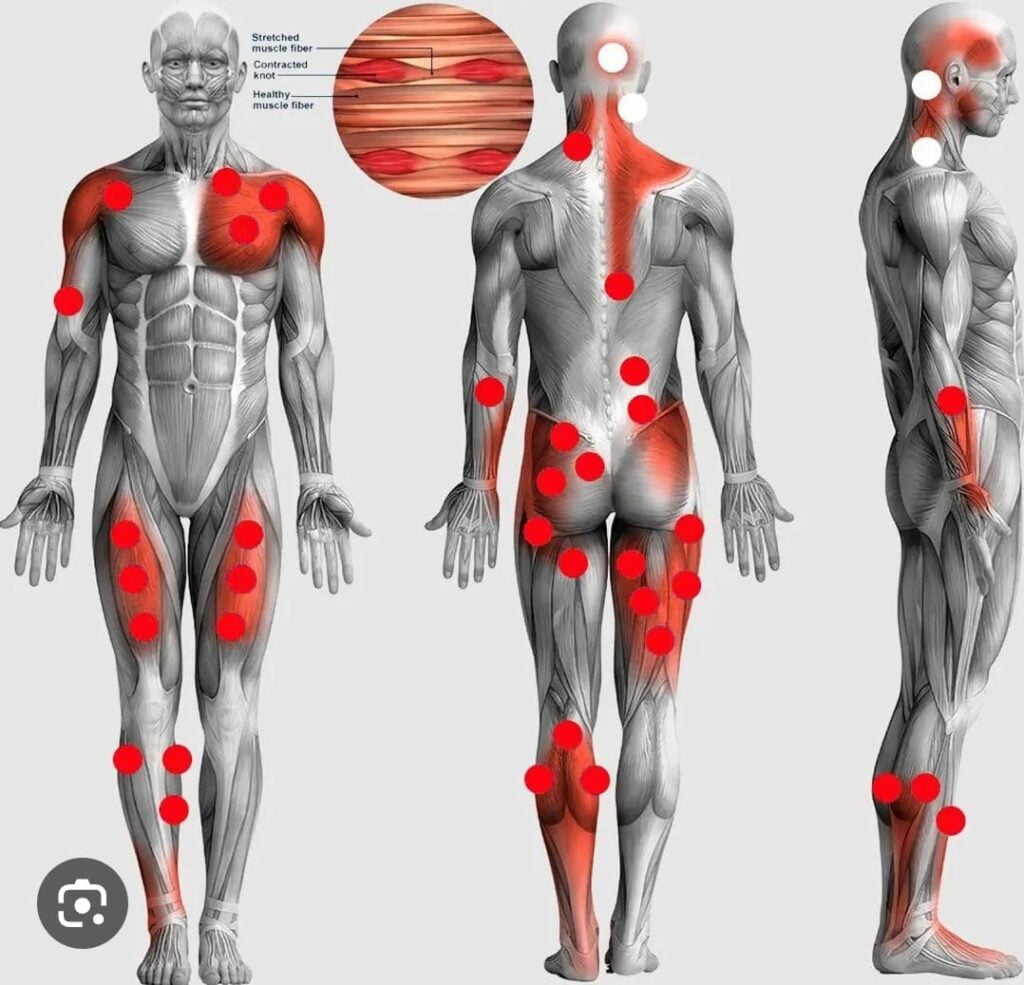
What is a Muscle Knot and How we can treat it?
The medical term for muscle knots is myofascial trigger points. These are occur when muscle fibers or the bands of tissue called fascia underneath them tense and tighten. Symptoms: These knots can develop almost anywhere on the body where muscle or fascia is present. The knots feel as if they are small, hard lumps or nodules. A person may have to press deep into their connective issue to feel the knots or trigger points. These knots commonly occur calf muscles, lower back, neck, shins, shoulders. Causes: Common causes of muscle knots include: Stress and tension, injuries related to lifting and repetitive motion, poor posture, prolonged bed rest or sitting without stretching. A person who spends a significant amount of time sitting at work may develop muscle knots due to staying in the same position for prolonged periods. sedentary lifestyle. People who play sports or work with their hands may also be at risk because they engage in repetitive activities. Repeatedly, doing the same motion can cause tension and knots over time. How to treat at home? People may want to try home remedies, which are often the first line of treatment for muscle knots. The individual should begin by evaluating why their muscle knots might have occurred. If someone’s muscle knots are due to prolonged sitting or a prior muscle injury, engaging in regular stretching breaks may help reduce muscle tension. People can also try: Applying a cloth-covered heat pad or ice pack to the affected area. Aerobic exercise, such as swimming, jumping jacks, and cycling to loosen tight muscles. Taking anti-inflammatory medications, such as ibuprofen to reduce muscle pain. If stress is the cause of someone’s muscle knots, they can take steps to reduce it, including: Taking short stretching and deep breathing breaks during the day Exercising for 30 minutes a day Reading a book or listening to music Getting more sleep at night Spending at least 15 to 30 minutes a day on relaxation techniques, such as meditation or gentle yoga
READ MORE3 Apr
Rocker bottom shoes
Rocker bottom shoes help strengthen back muscles, reduce low back pain Sports Physiotherapy- Researchers of the Sports Physiotherapy master’s degree at Valencia’s CEU Cardenal Herrera University have confirmed, in a new study of their research work into back pain, that unstable shoes improve the strength of back muscles in order to maintain balance and stability when walking. Forefoot Rocker Sole: A rocker placed just behind the metatarsal heads is much effective at reducing pressure under the ball of the foot and reducing motion in the toe joints. Thus we use it for treating hallux limit us (big toe arthritis) and ball-of-foot pain. Physiotherapy Horsham, Physiotherapy East Grinstead. Heel to Toe Rocker Sole: This type of rocker sole has the thickest point farther back on the shoe. This type of rocker shoe can be effective for limiting ankle and midfoot movements. Thus, it is helpful when a patient has ankle arthritis or midfoot arthritis. It also can reduce pressure on the heel at heel strike, as the foot rolls faster off of the heel. To contact our Physiotherapy clinic in Horsham or Physiotherapy in East Grinstead please contact us on info@anrc-uk.com, www.anrc-uk.com ANRC Physiotherapy clinic deals with Sports physiotherapy, MSK physiotherapy, and domiciliary physiotherapy How to self-manage foot pain and swelling Try these things for a week: If you can, avoid standing on it-put as little weight as possible on the foot Apply an ice pack (or a bag of frozen peas in a towel) on the foot for up to 20 minutes every 2 to 3 hours Wear comfortable shoes – for example, avoid shoes with heels Take paracetamol
READ MORE7 Jan
Treatment for Anterior Knee Pain- Physio Horsham
Physio Horsham-Patellofemoral pain, also referred to as anterior knee pain, is a common musculoskeletal condition in the general and sporting communities. Anterior knee pain affects up to 25% of the population, 36% of adolescents and is more prevalent in females. Patellofemoral Pain Syndrome is categorized by anterior or peri-patellar knee pain in the absence of other knee pathology. This pain can be diffuse or sharp and is usually associated with at least two of the following activities in day to day life: Squatting Ascending or descending stairs Kneeling Sitting for long periods Walking/running Diving It may be associated with crepitus on knee movements, occasional swelling particularly after exercise, and pseudo locking or giving way. An injury might happen in the past also can be a reason. Role of physiotherapy in Knee pain-Physio Horsham Physiotherapy is the mainstay of conservative treatment for this condition and the Chartered physiotherapy profession has received international recognition for anterior knee pain management. The most effective treatment for patellofemoral pain is a McConnell program, designed and monitored by a physiotherapist according to the patient’s individual needs. This recognized anterior knee pain management program was first introduced by Jenny McConnell, an Australian physiotherapist (McConnell, 1986). The approach uses a specialized, functional exercise program to improve the muscle control around the knee and taping to reposition the patella. In association with electrotherapy modalities. What can gain by physiotherapy? When treatment is given by a physiotherapist trained in patellofemoral pain, the results are excellent. In the majority of patients, only five to six treatments are required to enable the patient to return to normal and sporting activities. Physiotherapy management, based on that described by McConnell, has been shown to be effective in two large case-series (McConnell 1986, Gerrard 1989) with up to 91% of anterior knee pain patients having an excellent or good response. Physiotherapists are currently undertaking the first randomised, controlled trial evaluating the effectiveness of this treatment compared to a placebo control. This project is being funded by the physiotherapy profession via the Physiotherapy Research Foundation. References McConnell J (1986): The management of chondromalacia patellae: A long-term solution. The Australian Journal of Physiotherapy 32(4): 215-223. Gerrard B (1989): The patellofemoral pain syndrome: A clinical trial of the McConnell program. The Australian Journal of Physiotherapy 35(2): 71-80. Finding a Physiotherapist Would you like the names of physiotherapists who have a special interest in McConnell Treatment for Anterior Knee Pain Contact us on info@anrc-uk.com 01342537610, www.anrc-uk.com
READ MORE6 Jan
Wry Neck
The term “wry neck” describes a condition whereby the neck suddenly becomes stiff and painful. Turning the head to the side (usually one side more than the other) and looking up can cause a severe “catching” pain. The muscles on one or both sides of the neck may also go into spasm and pain may be felt from the base of the skull right down to the shoulder blade and outwards to the top of the shoulder. WHAT CAUSES OF WRY NECK? There are various causes, the most common being: Poor sleeping posture such as positioning of pillows. A sudden flicking or jerking of the head. Viral Infections. Exposure to cold weather. TREATMENT OF WRY NECK In most cases, if treated immediately by the physio, wrynecks respond exceptionally well to treatment in 3-4 days. Mobilisations and heat are applied to loosen the neck joints and reduce the pain and muscle spasm. HOME TREATMENT FOR WRY NECK Don’t: Go out in the cold without being well appropriate clothes. Hold the neck still or overprotect. Sit or lie with the neck in an awkward position Do: Keep warm. Use a hot water bottle wrapped in a towel or hot showers for pain relief. Keep your neck moving within the pain-free range. Take pain medication if your pain is severe. FOR FURTHER INFORMATION see your local Physiotherapist. Click here to https://anrc-uk.com/physiotherapyfind your closest ANRC Physio clinic FOR MORE INFORMATION see your local Physio Practitioner. Click here to find your Physiotherapy clinic
READ MORE6 Jan
Suffering from Cervicogenic Headache?
Suffering from Cervicogenic Headache? There is widespread support in the literature that headaches are often multifactorial in their origins. If your assessment reveals poor posture, knots within the muscles, previous history of RTA, limited range of cervical spine movement, palpatory tightness or a reproduction of symptoms on cervical palpation you may consider referring to physio. Even a short trial period of treatment is often used to help with differential diagnosis provided medical review is arranged if symptoms remain unchanged. PHYSIOTHERAPY TREATMENT Treatment is guided by signs and symptoms but the literature supports a 2 phase programme: Mobilisation of the upper cervical spine Improvement in symptoms of a cervicogenic headache has been shown with attention to pain provoking structures (Edeling 1994, Jull 1994b, Schoensee 1995). However, whilst improvements were gained in the short term there was a plateau after mobilization. Muscle Re-Training Specific exercises isolating the deep flexors and addressing postural dysfunction. In a study by Beeton and Jull(1994) it was found by incorporating these into a more comprehensive programme that improvements were maintained 6 weeks after treatment had ceased. References: Edeling J (1994): Manual Therapy for a Chronic Headache (2nd ed.) Oxford: Butterworth- Heinemann.*Jull GA(1994b): Headaches of cervical origin. In Grant R(Ed.): Physical Therapy of the Cervical and Thoracic Spine (2nd ed.) New York: Churchill Livingstone). Schoensee SK, Jensen G, Nicholson G, Gossman M and Katholi C (1995): The effect of mobilization on cervical headaches. Journal of Orthopaedic and Sports Physical Therapy 21(4): 184-196. Our client feedback ClaireH-98 17 Aug 2016 – Relief After 25 Years Having suffered from headaches for 25 years (and tried all sorts of unsuccessful treatments), I heard about trigger point therapy and decided to give it a go. The intense hands-on physiotherapy freed my neck and back up and reduced the severity of my headaches. Praveen gave me a number of short exercised to facilitate improvement and I found that combining these with his treatment has brought much relief from pain. I would highly recommend this treatment and in particular, Praveen who is very experienced and very pleasant. East Grinstead Physiotherapists are involved in a comprehensive ongoing education programme including the management of acute and chronic headaches. FOR MORE INFORMATION see your local Physio Practitioner. Click here to find your Physiotherapy clinic
READ MORE5 Jan
Physio East Grinstead
Physio East Grinstead Physio East Grinstead is the predominant allied health group within the ANRC Physio network. Physiotherapy is a science-based healthcare profession that views the human movement as central to Well-being and Health. Physio aims to maintain and restore human function after disease or any injury, to help people achieve the quality of life through physical movement and strength. East Grinstead Physiotherapists are highly trained to assess and diagnose your condition, then plan and administer treatment programs to restore function to the highest possible level. ANRC Physiotherapists also work in partnership with Doctors and other health professionals to ensure the best possible treatment and care. Using a combination of manual therapy, trigger point therapy, therapeutic exercise, education, lifestyle advice, workstation assessments, Ergonomics assessments soft tissue techniques, and electro-physical modalities, ANRC Physiotherapists strive to enhance health and maximise the potential of the service users. Physiotherapy brings relief to people of all ages, in reducing pain and improving mobility. Restoration of normal body posture and alignment can lead to a speedy recovery and prevent recurrence of the problem. Physiotherapy is suitable for all disorders that have the symptoms of pain, stiffness, loss of movement and weakness. The following benefits can be gained with physiotherapy. What to expect when you visit a Chartered Physiotherapist in private practice physiotherapist will first take a detailed history of your condition together with any relevant past medical history A physical assessment will then be undertaken to determine the clinical diagnosis of your problem. The physiotherapist will discuss with you a proposed treatment plan and will give you an estimate as to the length of treatment required and the probable outcome of your treatment. Physiotherapy is beneficial for conditions such as: Back and neck pain Sports massage Indian Ayurveda relaxation massage Headaches Sports Injuries Muscle and joint pain Post-operative, acute or chronic injury Arthritis Posture and alignment problems Osteoarthritis knees Sciatica Adolescent and children’s injuries AFTER HOURS ANS SATURDAY APPOINTMENTS AVAILABLE We are located ANRC Physiotherapy Clinics East Grinstead – Judges Cl, East Grinstead, West Sussex, RH19 3AA
READ MOREQuick Contacts
- Phone : +44 7483 807551
- Email : info@anrc-uk.com
- Locations : Horsham, East Grinstead, Ashurstwood, Lingfield
- Country : United Kingdom